2012 Rollins PhD student cohort
Public Health Research into Action
Monday, December 17, 2012
Friday, November 30, 2012
Say Goodbye to Third-hand Smoke
Do you remember the smell when a
smoker gets in an elevator after enjoying a cigarette, or in a hotel room where
people were smoking? Is what you smell bad for health? Scientists tell us
“Yes”, for it is so toxic that even our nose is telling us to get away.
This is the so-called “third-hand
smoke”, invisible yet toxic brew of gases and particles clinging to smokers’
hair, skin, and cloth, or carpet, cushion, and furniture in a room, or seats in
a car, or simply dust. Residue from tobacco smoke adsorbs to nearly all
surfaces long after a cigarette has been quenched, and can persist there for
days, weeks, or even months. Certain chemicals in the residue, for example the nicotine, can further react with ambient air pollutants to form potent
carcinogens - chemicals that may lead to cancer, which makes the case even
worse.
Thus, staying in a room or car
today where people smoked yesterday is not good for health. This is especially true
for children and infants, as they can easily get the third-hand smoke on their
hands and ingest it when they are crawling on the floor and tasting fingers,
puppets, or cushions in an environment where people smoked. Simply avoiding
smoking in front of children, say smoking in your house or car when children
are out, can barely protect them from the harm. Smoking outside might be
better, but residue smoke may still cling to your skin and cloth, and then get
passed on to your children when you give them a big hug!
Sounds horrible, right? Then take
some actions!
1. Don’t
smoke inside your house or car. Simply closing the kitchen door, opening the
window, or turning on the fans won’t protect your children from third-hand
smoke!
2. Replace
nicotine-laden furnishings, carpets, and wallboard - this may reduce the
exposures.
3. If
you do smoke outside, clean your face and hands and get changed before playing
with kids. Don't give your kids a “smoky” hug!
4. The
easiest and hardest, and of course the ultimate way of getting rid of
third-hand smoke is: QUIT SMOKING! Create a smoke-free environment for you and
your beloved ones!
Wednesday, November 28, 2012
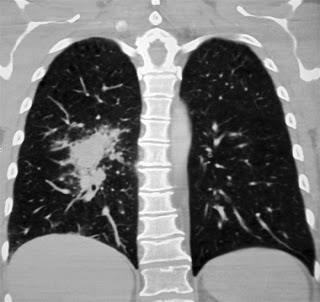
To screen, or not to screen?
The debate over lung cancer screening
Lung cancer is the leading cause of cancer related death
among both men and women. By the time most patients are diagnosed with lung
cancer, it is usually rather advanced and becomes difficult to treat. Detecting
lung cancer at earlier stages has the potential to make a significant impact on
death rates from the disease.
For years there was hope that chest x-rays would be an
effective screening tool, but several studies found it to be ineffective. As
imagining technology evolved, low-dose CT scans (LDCT) quickly becomes the most
promising tool to screen for lung cancer. Several studies have been conducted
to determine if using LDCT to screen for lung cancer would save lives. Results
from the National
Lung Cancer Screening Trial (NLST) found that among smokers and former
smokers who are age 55 to 74, have smoked for 30 pack years or more (pack years
are calculated by multiplying the number of packs a person smokes or has smoker
per day by the number of years they’ve been smoking, so thirty pack years would
be equal to a person who smoked a pack a day for thirty years, or 2 packs a day
for 15 years) and either still smoke or have quit smoking within the past 15 years,
yearly screening with LDCT can reduce their risk of lung cancer related death1.
 |
While these results are promising, there were also several drawbacks
and complications associated with LDCT that are equally important to take into
consideration. The images produced by LDCT will not only make tumors visible,
but also other benign, or non-threatening lesions, or spots. It’s been estimated that of those screened
with LDCT, 20% will screen positive and need some sort of follow-up2.
The required follow-up will consist of additional tests and surgical
procedures. These tests and surgical procedures all have their risks and could
result in potentially serious complications. Only 1% will actually have lung
cancer. The burden placed on those who
required follow-up, but turned out not to have lung cancer, is not trivial. Dr.
Herald Varmus, Director of the National Cancer Institute, was quoted as saying,
“There are economic, medical, and psychological consequences of finding these
abnormalities” to the New York
Times in an interview shortly after the results of the NLST were released.
Estimates from a national survey indicate that approximately
8.7 million Americans would be eligible for lung cancer screening with LDCT
based on the results of the NLST3. At a cost of about $300 to $500
dollars per LDCT2, there is some concern that screening this many
people could overwhelm the healthcare system.
Without an official guideline, it’s unclear if insurance will cover the
screening test. Also, the eligibility criteria for screening are rather
complicated and may not be well implemented, likely resulting in unnecessary
screening. There is also concern that the availability of a screening test for
lung cancer will give smokers a reason not to quit.
Additional analyses and studies will need to be conducted in
order to determine if lung cancer screening with LDCT is viable and safe. In
the mean time, avoiding
smoking or quitting altogether remains the most effective way to prevent
lung cancer and not have to worry about lung cancer screening.
Juan Rodriguez is a doctoral student in Behavioral Science
and Health Education at Emory University. He is an avid watcher of the reality
TV show Hoarders because he lives in fear that his wife will one day become a
hoarder.
Sources
1 – National Lung
Screening Trial Research Team. (2011) Reduced Lung-Cancer Mortality with
Low-Dose Computer Tomographic Screening. New England Journal of Medicine.
365(5):395-409.
2 – Bach PB, Mirkin
JN, Oliver TK, Azzoli TK, Berry DA, Brawley OW, Byers T, Colditz GA, Gould GA,
Jett JR, Sabichi AL, Smith-Bindman R, Wood DE, Qaseem A, Detterbeck FC. (2012)
Benefits and harms of CT Screening for Lung Cancer: A Systematic Review. JAMA.
307(22):E1-E12.
3 – Doria-Rose VP,
White MC, Klabunde CN, Nadel MN, Richards TB, McNeel TS, Rodriguez JL, Marcus PM.
(2012) Use of Lung Cancer screening tests in the United States: Results from
the 2010 National Health Interview Survey. Cancer Epidemiology, Biomarkers and
Prevention. 21(7):1049-1059.
Is math killing you?
If you are a student, or know someone who is, you are well aware that it's that time of year where final exams and papers are in full force. You've probably also heard desperate sighs followed by "my math class is killing me".
Sounds crazy, right? Maybe not. That stomach ache that you get every time you think about your math class may not be "all in your head". A new study has found that anticipation of math-related tasks can stimulate a part of the brain associated with threat detection (think fight or flight response) and may actually result in actual experiences of pain. Although this "pain" won't actually kill you, according to Lyons and his team, this pain response may explain why some people tend to avoid math and math-related situations.
Awesome, as if you need another reason to dread that math exam. The good news is that anxiety in anticipation of math was not actually related to performance, so don't despair! Being worried about that homework or final doesn't mean that you should give up all together!
Instead, explore ways to reduce your anxiety so that you can stay health and focus on the task ahead. There is no one right way to de-stress, so be open to the possibilities and find what works best for you!
In the classroom, try different approaches to learning the material, like trying new ways of studying, talking with your professors and peers or getting a tutor. Some people may even find that some medications, like beta-blockers, make stressful situations more manageable.
Consider embracing your fear. Mindfulness-based mediation, a type of meditation based in Buddhist principles may be a promising way to control physical and emotional pain. This type of meditation is all about being present in the moment and raising your awareness in a nonjudgemental way. Perhaps one of the best ways to get rid of your anxiety is to get to know it!
At home, explore different ways of relaxing in general, like yoga, going for a walk, or enjoying a good meal with friends. Chances are, you have things you like to do when you are not studying or working, so be kind to yourself and allow yourself the time to recharge so that your mind is fresh and you can focus on learning.
And most importantly, don't give up!
Who knows, maybe you are the next Albert Einstein.
Danielle Haley is a doctoral student at Emory University in the Department of Behavioral Sciences and Health Education. She is currently dealing with her own math-related stress by riding her horse, Luna.
A Bad Start with a Promising End: HIV and HPTN 052
The rumor mills were in full
force to fill the gaps. Eventually,
rumor gave rise to fear and AIDS made its way from the obituaries to the front page. In 1987, the house of local family with three
HIV-positive sons was set ablaze.[1] The
news was shocking: How could anyone do this?
Was AIDS so feared that neighbor could be pitted against neighbor in
blind efforts to control it? The news
made many of us doubt if AIDS could ever be viewed in the same light as other diseases
as cancer and diabetes.
In 1996, good news came in the
form of a group of medications called anti-retroviral therapy (ARVs). This news gave hope to ending what was then considered
the worst disease imaginable. It gave optimism
to people who were otherwise destined to die. With ARVs, a diagnosis with HIV/AIDS could no
longer be viewed as fatal, but rather a manageable, long-lasting illness.
Test and Treat?
Fast forward to May 12,
2011. On this day, results of the HPTN 052 clinical trial
announced that if a heterosexual, HIV-positive person continually takes their ARV
medications, the risk of transmitting HIV to their sexual partner could be
reduced by 96%.[2] In other words, HIV-positive people
taking ARVs were more than 20 times less likely to infect their partners than
untreated people. The study was groundbreaking. In the words of UNAIDS executive director,
Dr. Michele Sidebe, the HPTN 052 findings were a definite “game changer” in how
we thought of HIV prevention.
The news of HPTN 052 brings new hope in the nearly 30 year
fight against HIV. Now, we can no longer
think of AIDS an incurable disease and actually start imagining what an “AIDS
free generation” could look like. Still,
we must not disregard the difficult days of 20 years ago. We should be reminded of the images that
plagued our newspapers and news broadcasts—images of young men dying from
AIDS-related causes, children thoughtlessly assuming that AIDS was death, and
communities turning against each other for fear of the disease.
Ray is a Doctoral Candidate in Health Policy and Management at Emory University. He has previously worked with several multinational organizations in Zambia and Thailand on programs related to HIV and TB care/treatment.
[1] "Arson Cause Of Fire At Rays -- Boys Start School Today" Orlando Sentinel, September 23, 1987
http://articles.orlandosentinel.com/1987-09-23/news/0150050182_1_andy-ray-ray-family-varnadore
[2] “Prevention of HIV-1 infection with early antiretroviral therapy.” http://www.hptn.org/research_studies/hptn052.asp
Subscribe to:
Comments (Atom)